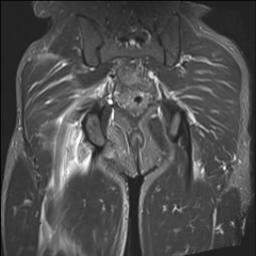
Proximal hamstring tears
Proximal hamstring tears typically occur with a violent event, such as playing sport or waterskiing. Patients will feel a tear, and there is usually a large amount of bruising, swelling and difficulty walking.
This injury can be missed. Typically an ultrasound will diagnose the proximal hamstring injury, which can be confirmed by MRI. However, as time is critical if surgical repair is considered, referral should NOT be delayed by waiting for an MRI, or the MRI should be performed on an urgent basis.


Patients who do not run or play sports may not require surgery. Those who do, and who present 2 – 6 weeks after surgery may consider surgery. This surgery is performed open, with the tendon mobilized, and repaired back onto the bone using suture anchors.
Postoperative rehabilitation
Proximal hamstring surgery is performed as day surgery at Women’s College Hospital. Someone must come and pick you up and take you home. It is advised to have someone around to help you for the first two days. All patients will be provided with a script for medications that should be filled at the hospital prior to going home. Medications will usually be Tylenol regularly for the first week, with a script for oxycodone also provided. Patients need to take a medication to reduce the risk of DVT/PE – typically Rivaroxaban 10mg once daily for 2 weeks.
All patients will wear a brace and use crutches for 8 weeks after surgery. After the brace comes off, patients can fully walk on the leg but may need crutches for a further 6 weeks – this depends on the duration of time between injury and surgical repair. Physiotherapy begins at 8 weeks, once the brace is removed.
Patients are seen in clinic two weeks after surgery, for wound review.
Patients should take a week off work after the surgery, and work from home for another 2 weeks if able. Patients are not allowed to play sport for 6 months after surgery.
Risks of surgery
Proximal hamstring repair is major open surgery, with a 1/100 risk of deep infection, major stiffness, DVT/PE, and major nerve or blood vessel damage. Patients can get local areas of numbness around the incision, and down the back of the leg – this typically improves over a year or two.
The major risk of the surgery is injury to the sciatic nerve which is very close to the injury. The risk of nerve injury (resulting in difficulty moving the foot) is 1/100.
Because of the risk of DVT / PE, patients must take a blood thinner after surgery – this raises the risk of bleeding or hematoma after surgery.
Rehabilitation can be difficult after this surgery. The risk of retear after surgery is approximately 5%.
If patients are treated without surgery, they typically achieve function of 70 – 80 out of 100. With surgery, if there are no complications, a function of up to 95/100 can occur.
