Hip arthroscopy
Patients with labral tears of the hip, or femoroacetabular impingment (FAI), are usually 16 – 50 years of age, and have pain in the groin. This pain is noticed with sporting activities, or with deep flexion such as sitting in a chair, or squatting.
The majority of patients do not report an injury which preceded their hip pain, leading many surgeons to believe that there is an anatomical problem around the hip (such as too much bone) which causes the labral tear, and subsequent hip pain.
It is important to manage these conditions initially with good physiotherapy and core exercises. Intra-articular injections of cortisone are often used, but seldom provide long term relief. They can however be useful to determine if the pain is coming from the labral tear, or from another source.
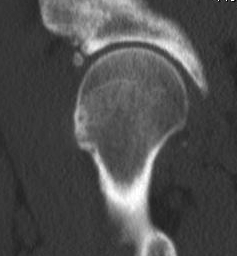
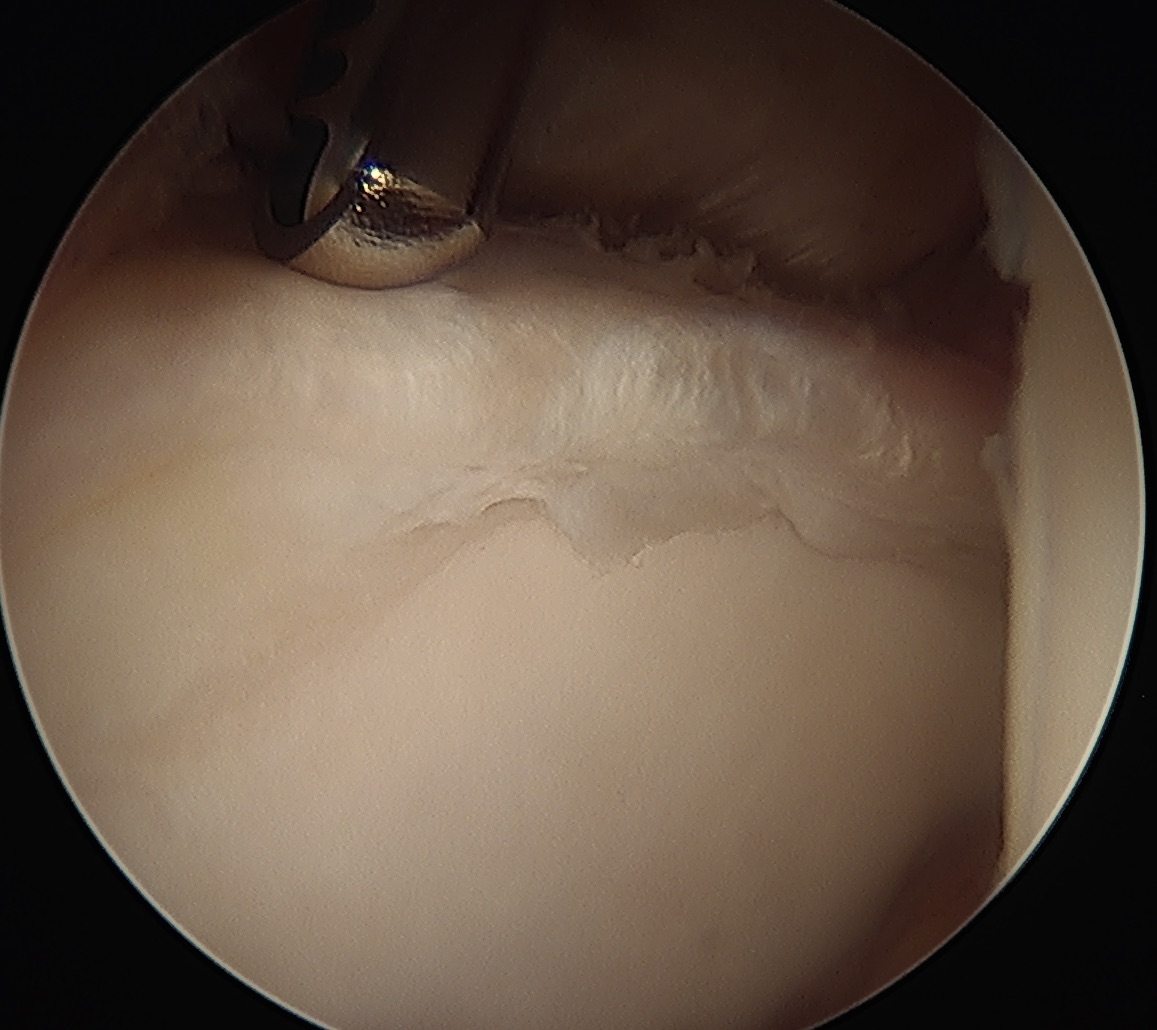
An MRI is very accurate at diagnosing a labral tear and any extra bone which may be contributing to the problem, such as a CAM (extra bone on the femoral side) or pincer (extra bone on the pelvis or acetabular side). Even more importantly, an MRI will look at the cartilage covering the femoral head (ball) and the acetabulum (socket). If you have significant cartilage damage, it is likely that a hip arthroscopy will not help. In this setting, injections of PRP or Hyaluronic acid may be used to treat your pain. Otherwise, a total hip replacement may be required.



If you have had debilitating pain for more than a year, and physiotherapy is not helping, hip arthroscopy may be an option. Other options include Hyaluronic acid (which can help for up to 6 months) and PRP (which can help for up to a year).
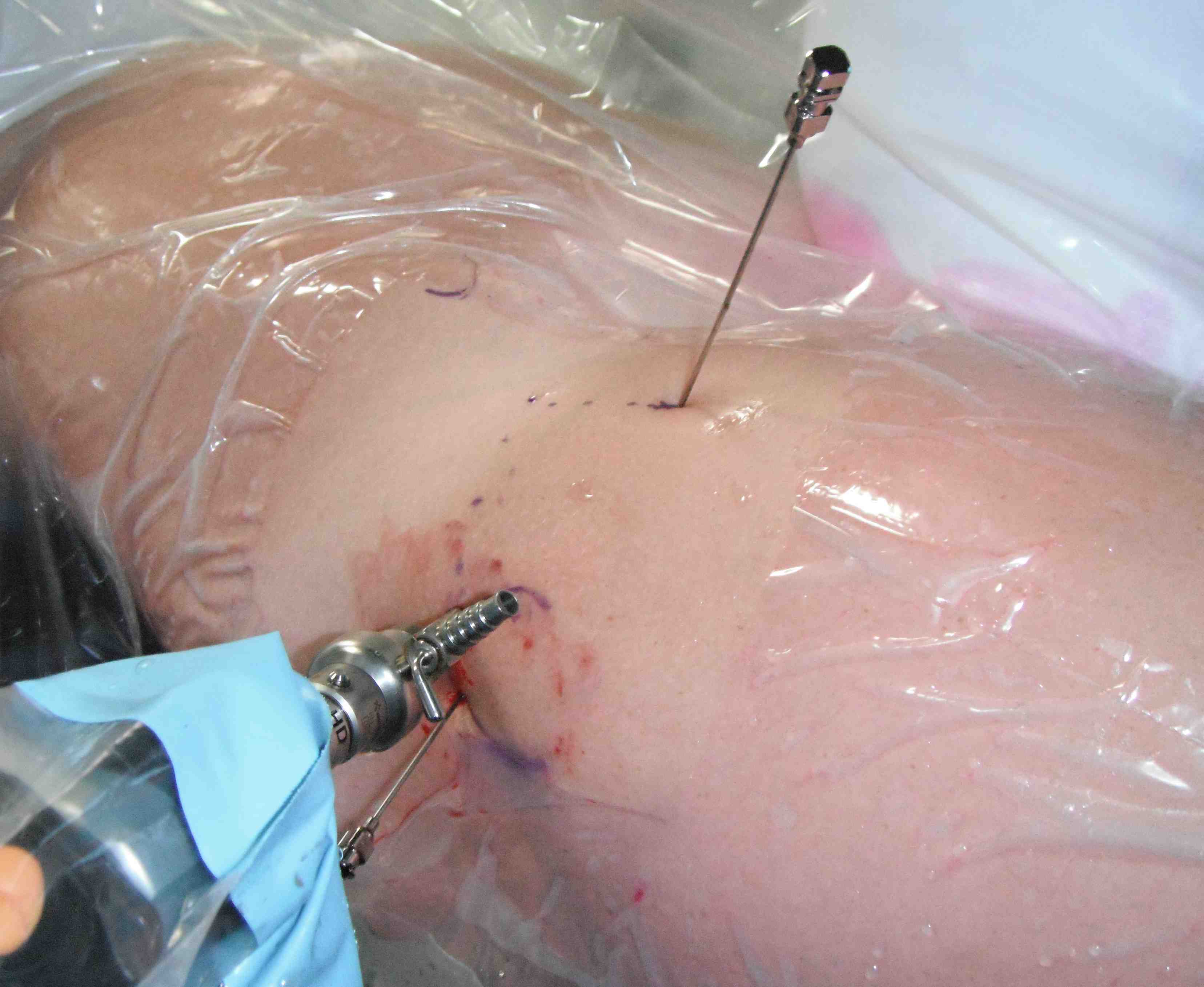
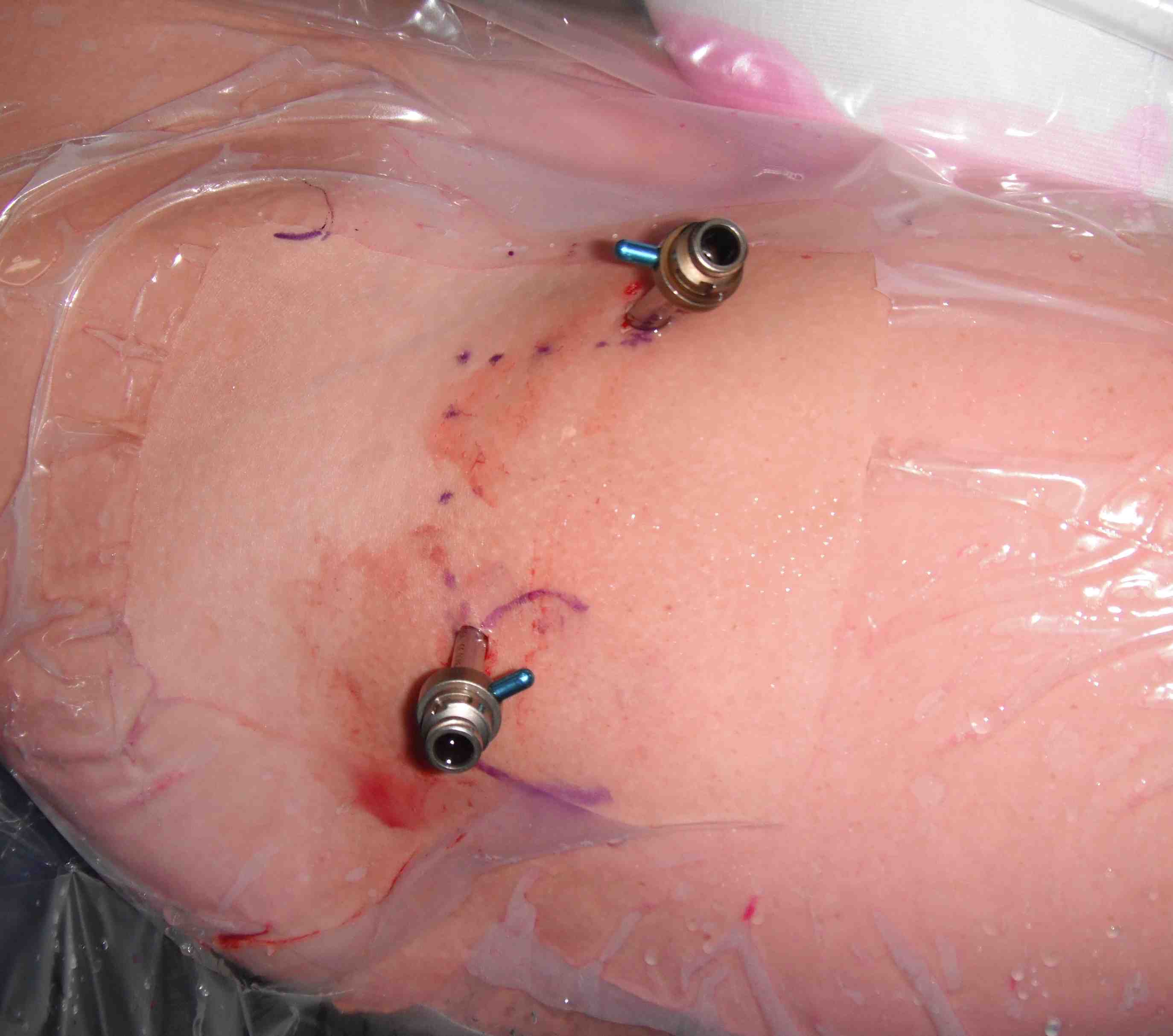
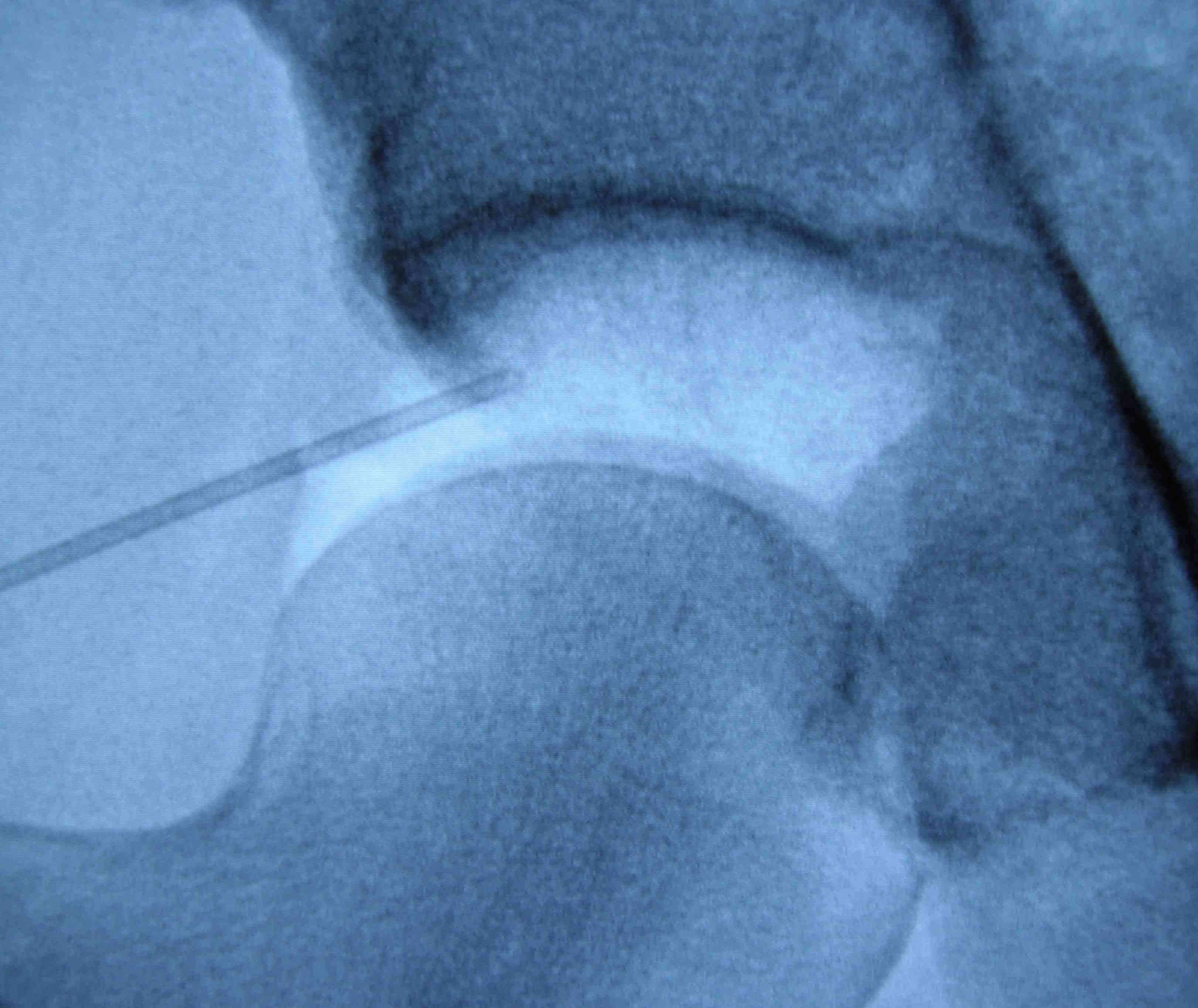
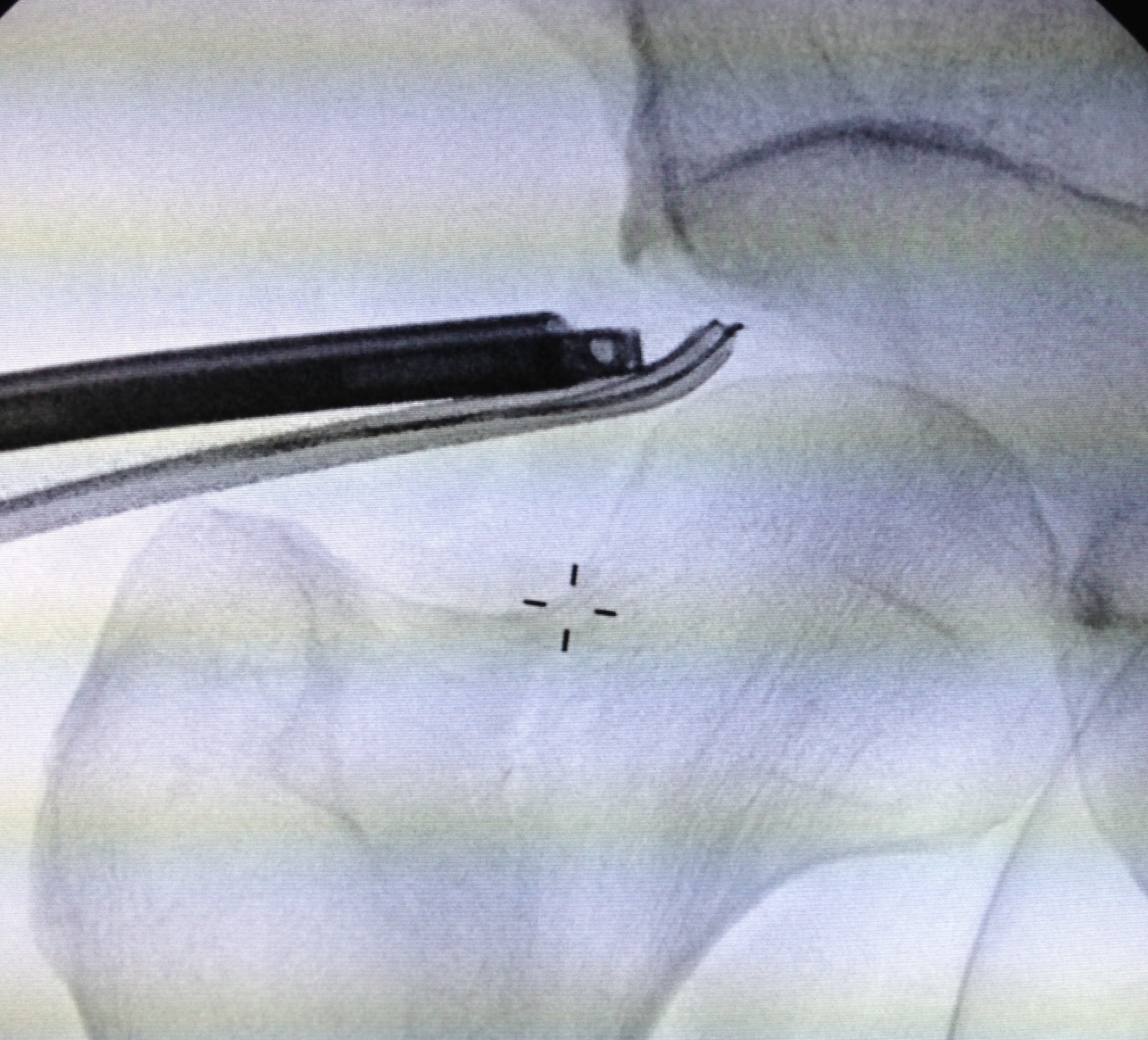
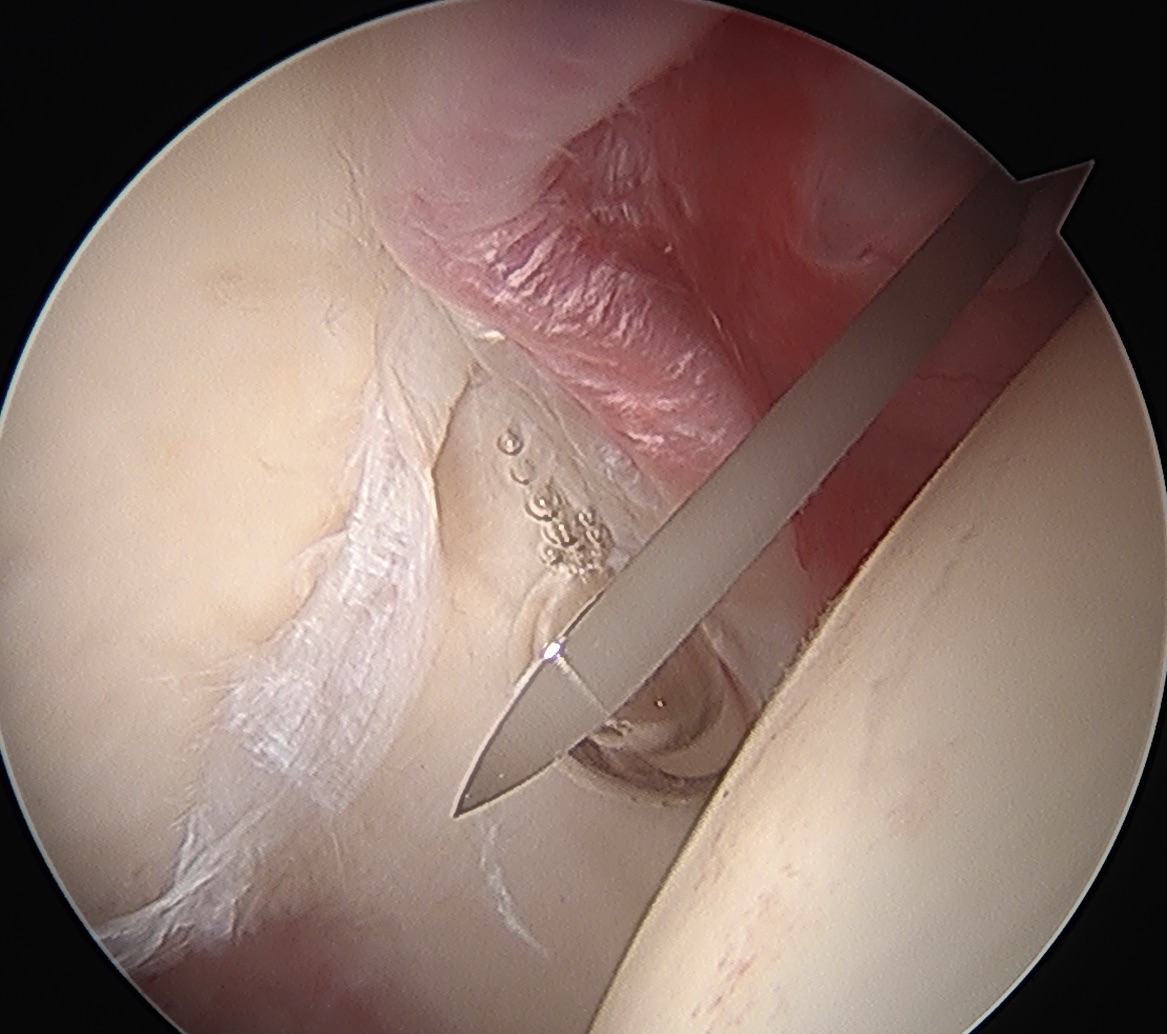
During this keyhole procedure, anchors with sutures are used to repair the labral tear. Extra bone is taken away from the acetabulum and the femoral head / neck area as needed. Usually the hip capsule is opened to access the hip joint fully, and this is carefully closed at the end of surgery.

Postoperative rehabilitation
Hip arthroscopy is performed as day surgery at Women’s College Hospital. Someone must come and pick you up and take you home. It is advised to have someone around to help you for the first two days. All patients will be provided with a script for medications that should be filled at the hospital prior to going home. Medications will usually be Celebrex in the morning for 2 weeks, Aspirin at night for two weeks, and Tylenol regularly for the first week. A script for oxycodone will also be provided.
All patients will be on crutches for 4 weeks after surgery. Physiotherapy begins immediately after surgery – a script and protocol will be provided for you.
If possible, patients should rent a Gameready machine, which provides ice and compression to the knee, significantly reducing postoperative pain. The information for the rental company will be provided to you. Patients are seen in clinic two weeks after surgery, for wound review.
Patients should take a week off work after the surgery, and work from home for a further 2 weeks after that if possible. Patients are not allowed to play sport for 6 months after surgery.
Risks of surgery
Hip arthroscopy is a relatively safe operation. The risk of major complication such as deep infection, hip fracture, hip dislocation, major nerve injury or DVT/PE is 1/1000.
Because the hip needs to be pulled out of joint by 1 cm, patients can get numbness in the groin or on the foot – this typically resolves over 6 weeks and is said to be permanent in 1/1000. Patients can get local areas of numbness around the incision and down the thigh – this can take a year to improve.
The chance that you will have a good outcome (80 – 90% improvement) is in the order of 80%, if your cartilage is normal. Patients can continue to improve for up to 12 months after surgery.
If you are in the 20% of patient that don’t have a good outcome, further investigations will be ordered such as a xray, CT and MRA to determine if there is a cause of your ongoing issues. However, often the issue is thought to be related to the orientation of your acetabulum, pelvis, and the way your spine and pelvis interact while walking, which is difficult to both diagnose and treat.
Potential causes of ongoing pain include labral re-tear, ongoing bony impingement, cartilage damage, capsular adhesions and capsular tears or defects.
